Is Post orgasmic illness syndrome (POIS) a urogenital disease or a psychiatric condition?
Post Orgasmic Illness Syndrome (POIS) is a rare urogenital disease characterized by the appearance of flu-like symptoms (fever, extreme fatigue, myalgia, itchy burning eyes, nasal congestion/rhinorrhea), as well as mood changes, irritability, and concentration, memory, and attention difficulties, within a few minutes to a few hours after ejaculation. Symptoms disappear spontaneously 3-7 days after onset.
Waldinger and Schweitzer first described POIS in two heterosexual male patients in 2002. Since then, around 70 cases with a professional diagnosis have been reported in the literature, plus around 430 self-reported. The prevalence of POIS is unknown, although there are over 1000 members of POIS patients noted in the American Internet forums: https://poiscenter.com, https://www.thenakedscientists.com, https://www.facebook.com/groups/145700934120948.
POIS is listed as a rare disease by the American National Institutes of Health and the European Orphanet. It is thought to be underdiagnosed, misdiagnosed, and underreported.
POIS seems to affect mostly men of various ages and relationship statuses worldwide. In 2016, the International Society for the Study of Women’s Sexual Health (ISSWSH) listed the Female Orgasmic Illness Syndrome (FOIS) among the new nomenclature of female sexual dysfunctions. Although the syndrome has been defined, the FOIS is based on expert opinion, as published reports and case series relate only to men, with only one documented female patient.
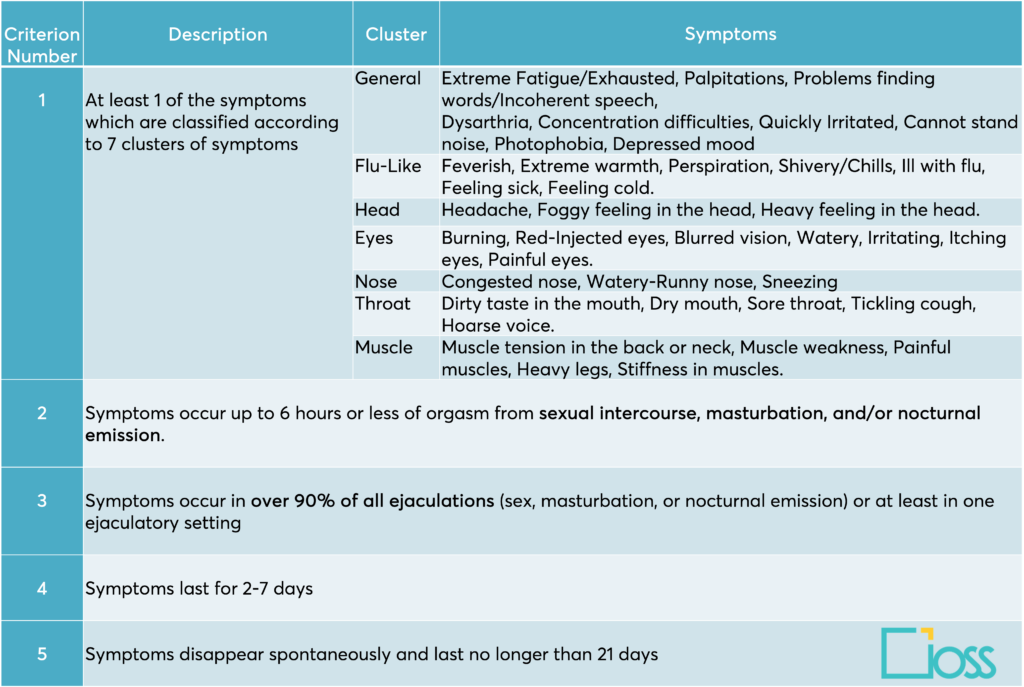
The most recent criteria are presented in the following table:
Although not all the patients satisfied each of the five criteria, most patients met three or more. Applying three or more criteria is suggested to achieve a higher probability that patients suffer from POIS. Prognostically, the available results indicate that these diagnostic criteria may not be independently helpful in predicting outcomes.
Clinical presentation
The distinguishing characteristics of POIS are:
- The rapid onset of symptoms after ejaculation
- An overwhelming systemic reaction (the so-called “POIS attack”) that includes a combination of several symptoms from different clusters.
In some men, the onset of POIS is in puberty (primary type), while in others, the onset is later in life (secondary type), with no clear evidence of which type is more frequent. The age at presentation is highly variable; in the largest published surveys, the average age was at the beginning of their thirties, with a duration of the syndrome around 7.5 years. The number of diagnostic criteria patients satisfied showed limited correlation to disease burden items, although patients with general, head, and throat clusters are more likely to experience severe disease.
The most-reported comorbidity is lifelong premature ejaculation (IELT < 1 min, 14 to 56%). Other comorbidities include depression and anxiety disorder. Given that POIS is a distressing condition, it is still unknown whether patients with POIS develop anxiety or depression due to their syndrome or whether patients with depression or anxiety are more likely to be diagnosed with POIS.
POIS’s physical and psychological effects can significantly affect patients’ quality of life (QoL). To reduce symptomatology and manage their life, most POIS patients:
- Reduce the frequency of sexual activity
- Avoid sexual activity/ejaculation
- Dampen eroticism and romance
- Schedule their sexual activity/ejaculation for times when they can rest and recover for several days afterward
- Lose pleasure and satisfaction
- Lose sexual intimacy
- Feel guilty
- Don’t start a new relationship
POIS affects not only men but also the QoL of their partners. Avoidance of sexual intercourse, dissatisfaction, distress, anger, and decreased intimacy are all described in the studies that evaluated this aspect. It was found that 10% of the patients divorced during follow-up because of avoiding sexual intercourse.
Physiopathology
The cause of POIS is unknown. Different pathogenetic mechanisms have been proposed, but none of them fully explain the disease. The following are the most accredited:
- POIS is an auto-immune or allergic disorder (Type-I and Type-IV) that causes an inflammatory reaction to a substance in the human seminal fluid.
- POIS is an auto-immune reaction to substances released during ejaculation, such as cytokines, prolactin, noradrenaline, etc. (disordered cytokine or neuroendocrine response).
- A hormone imbalance, such as low progesterone, low cortisol, low testosterone, elevated prolactin, hypothyroidism, or low DHEA, causes POIS.
- A disorder of endogenous opioid receptors causes POIS as symptoms mimic opioid withdrawal, and the orgasm mechanism consumes large amounts of endogenous opioids.
- POIS may be due to hypersensitivity with transient dysregulation of the autonomic nervous system, with parasympathetic over-reactivity, releasing mast cell mediators that can provoke postcoital asthma and/or rhinitis.
The causes of POIS likely differ in different individuals. POIS could represent “a spectrum of syndromes of differing causes”. None of the proposed causes for POIS fully explain the connection between POIS and lifelong premature ejaculation.
As there is no consensus on the underlying aetiology of POIS, consequently, we still miss a recognized treatment protocol. Current treatment options aim mainly at symptom’s management and include antihistamines, nonsteroidal anti-inflammatory medication, immune suppressants, selective serotonin reuptake inhibitors, benzodiazepines, Alfa-blockers, testosterone therapy, and hyposensitization. The treatment choice should be guided according to the symptoms and in a shared decision process with the patient and the partner.
Bio-psycho-social Assessment & differential diagnosis
In clinical practice, patients need to be thoroughly examined in an attempt to find the causes of their POIS symptoms, which are often difficult to determine and vary across patients. Once a cause is hypothesized, an appropriate treatment can be tried. At times, multiple treatments are attempted until one that works is found. Patients suspected of having POIS should undergo a sexual interview about their complaints and sexual function, with attention to ejaculation disorders and traumas. The onset, course and length of symptoms must be well noted. Addressing the POIS’s effect on the patient and the relationship distress must complete the sexual history taking, as patients can suffer from their symptoms with considerable emotional and psychosocial strain. It is crucial to have a complete medical history, including current allergies, STI, chronic prostatitis, chronic pelvic pain, or LUTS. Clinically diagnosed males should undergo routine tests, including a full blood count and hormonal laboratory tests (FSH, LH, prolactin, and testosterone). Patients should be carefully examined and screened for other diseases with POIS-like symptoms, such as post-orgasmic cataplexy, orgasmic headache, post-orgasm sneezing and rhinorrhea, postcoital dysphoria, post-coital asthma and rhinitis, Dhat syndrome. A neuropsychiatric evaluation is also recommendable to evaluate potential neurological or mental conditions.
Without recognized physical causes, symptoms can often be dismissed as psychogenic. Although it is reasonable to explore psychological issues triggered by sexual activity, such as guilt, religiosity, prior sexual abuse, or feelings of uncertainty about sexual orientation or gender identity, evidence in this piece of assessment doesn’t have to mislead the diagnosis of POIS. Health Care professionals should remember that a man may feel embarrassed and ashamed to discuss his symptoms openly. Although little is known about this syndrome, formally recognizing the symptoms as POIS reassures patients that they are not suffering from a psychiatric, psychosomatic, or other unknown disorder.
Back to our question
As usual, when we do not know the cause of a disease, we tend to attribute symptoms to a psychogenic condition. POIS doesn’t seem to escape this bad habit. Although we are in the stage of collecting data on the diverse pathophysiologic mechanisms, with some good evidence on some of them, it seems that the majority of the patients are referred to psychologists or psychiatrists, who, on their side, always can find what applied to their hypotheses (in other words, to see what they expect to see), as there is so little awareness about this condition. So, POIS is prone to being erroneously ascribed to psychological factors such as hypochondriasis or somatic symptom disorder or to unresolved issues with intimacy or sexuality.
Is this coherent with the current knowledge of the disease? Clearly not. POIS likely has an organic base with which biopsychosocial factors influence specific distress.
Is a referral to a psycho-sexologist useful? Yes, if the professional is competent on the condition and can collaborate with the urologist for the patient’s and the couple’s well-being.
What is the state of the art? Unfortunately, limited information is available on POIS; therefore, many affected people do not seek medical help, and most professionals are unfamiliar with the syndrome and its impact on quality of life. Continuing education for practitioners and awareness of the population is needed. Adding a poster in our office could be a contribution to start. Clinically, patients satisfying some or all of the diagnostic criteria should merit suspicion for POIS, adequate evaluation, and treatment options. Symptoms improvement rate after treatment is still unsatisfactory, and not all the reports include a follow-up. We should ask ourselves if we put the best of our competence in managing these patients. What I realized from my clinical experience is that what gives some relief to patients is not the fact that we have the solution in our hands: this could be great, but sometimes we do not have clear answers. It’s mostly because they feel understood and not interpreted as mentally vulnerable if they’re not. It’s because we professionals show a genuine attitude and commitment to finding a way for them, questioning our hypothesis when they are not working for the specific case.
Francesca Tripodi
Main References
- Abdessater M, Elias S, Mikhael E, Alhammadi A, Beley S. Post orgasmic illness syndrome: what do we know till now? Basic Clin Androl. 2019;29:13.
- Natale C, et al. Analysis of the Symptomatology, Disease Course, and Treatment of Postorgasmic Illness Syndrome in a Large Sample. J Sex Med. 2020;17(11):2229-35.
- Nguyen HMT, Bala A, Gabrielson AT, Hellstrom WJG. Post-Orgasmic Illness Syndrome: A Review. Sex Med Rev. 2018;6(1):11-5.
- Parish SJ, et al. Toward a More Evidence-Based Nosology and Nomenclature for Female Sexual Dysfunctions-Part II. J Sex Med. 2016 Dec;13(12):1888-1906.
- Paulos MR, Avelliino GJ. Post-orgasmic illness syndrome: history and current perspectives. Fertil Steril. 2020 Jan;113(1):13-15.
- Reisman Y, Tripodi F. Post-Orgasmic Illness Syndrome (POIS), in Textbook of Rare Sexual Medicine Conditions, Springer, 2022.
- Reisman Y. Clinical experience with post-orgasmic illness syndrome (POIS) patients-characteristics and possible treatment modality. Int J Impot Res. 2021 Jul;33(5):556-562.
- Waldinger MD, et al. Postorgasmic illness syndrome (POIS) in 45 Dutch Caucasian males: clinical characteristics and evidence for an immunogenic pathogenesis. J Sex Med. 2011;8:1.
- Waldinger MD, Schweitzer DH. Postorgasmic illness syndrome: two Cases. J Sex Marital Ther. 2002;28:251–5.
- Waldinger MD. Post orgasmic illness syndrome (POIS). Transl Androl Urol. 2016;5(4):602-6.